Telehealth Reverse Diabetes And Restore Immune Function
COVID-19 threatens us all. So far, we haven’t found a completely effective treatment. We may not even be protected from illness after we’ve recovered from infection. Vaccination to protect us is at least a year away. What should we do in the meantime?
The natural response to infections involves immunity cells.
The metabolism of these cells is just as complicated as cells in any other system. They depend on sugar, fat and protein for energy to operate just like function in all other cells.
Insulin is especially important. Insulin resistance from poorly controlled diabetes damages immune function. Just like it damages function of muscle, liver, heart, brain and nerves.
Let us show you how to improve immune function. By reducing abdominal obesity and increasing physical fitness.
To learn more about programs Herd Healthcare offers, our website is:
www.herdhealthcare.com
We already know who has poor immune function. People with chronic diseases. But also, people with chronic conditions such as high blood pressure, obesity and diabetes. In fact, almost everybody could improve immune function. By improving nutritional fitness and physical fitness.
 Sound familiar? That’s the way to reverse and recover from type 2 diabetes. Here we have an opportunity to avoid severe COVID-19 illness right away and prevent disability with type 2 diabetes for the rest of our life.
Sound familiar? That’s the way to reverse and recover from type 2 diabetes. Here we have an opportunity to avoid severe COVID-19 illness right away and prevent disability with type 2 diabetes for the rest of our life.
Truly creative insight. An Aha! moment.
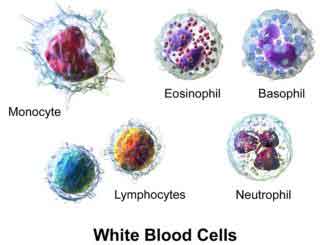 The immune system is a complex network of cells that defends the body against infection. These are white blood cells circulating in blood and specialized cells located in organs and tissues.
The immune system is a complex network of cells that defends the body against infection. These are white blood cells circulating in blood and specialized cells located in organs and tissues.
Immunity cells recognize chemical patterns of normal, healthy cells. They also recognize molecular patterns of unhealthy cells. Damage caused by physical injury or chemical poison causes immunity cells to isolate and remove unhealthy cells.
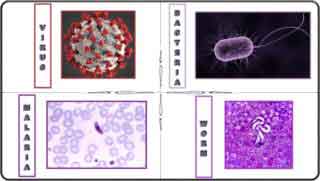 Infections by viruses, bacteria and invading organisms also stimulate an immune response. Viruses are large molecules that get attached and rely on living cells to function and reproduce. Bacteria are complete cells that can live on their own but rely on host cells to reproduce in large numbers. Other invading organisms include single-celled organisms like malaria that can live outside the body. Other organisms include worms that have many cells and can produce eggs that mature and live a long time inside or outside the body.
Infections by viruses, bacteria and invading organisms also stimulate an immune response. Viruses are large molecules that get attached and rely on living cells to function and reproduce. Bacteria are complete cells that can live on their own but rely on host cells to reproduce in large numbers. Other invading organisms include single-celled organisms like malaria that can live outside the body. Other organisms include worms that have many cells and can produce eggs that mature and live a long time inside or outside the body.
Chemical patterns of many infections cause a rapid response whenever they appear.
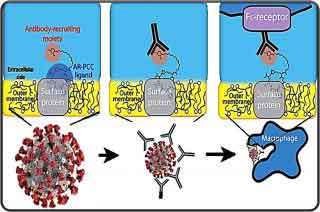 Other infections stimulate proteins that attach to invading molecules and structures. These proteins, called antibodies, recognize invaders and attach themselves to invaders. Once attached, antibodies change chemistry and destroy infected cells. Destroyed cells and invaders are taken from the blood by scavenger immune cells. Antibody production continues for as long as it takes to get rid of invaders. After recovery from infection, antibodies remain in blood and tissue for weeks, months or years. Guarding against reinfection.
Other infections stimulate proteins that attach to invading molecules and structures. These proteins, called antibodies, recognize invaders and attach themselves to invaders. Once attached, antibodies change chemistry and destroy infected cells. Destroyed cells and invaders are taken from the blood by scavenger immune cells. Antibody production continues for as long as it takes to get rid of invaders. After recovery from infection, antibodies remain in blood and tissue for weeks, months or years. Guarding against reinfection.
New antibody proteins are added to the network of cells and proteins that destroy infections. Any return of infection is quickly recognized and destroyed. Some antibody responses are retained for a few months or years and some are stored for response whenever some infection returns.
Overweight, obesity and type 2 diabetes damage immune response to infection. Immunity cells depend on normal metabolism of sugar, fat and protein just like cells in all other systems. When overloaded with sugar and fat, they become resistant to insulin.
Response to infection requires rapid action by immunity cells. This brings quick adjustments in metabolism stimulated by insulin. Overweight, obesity and type 2 diabetes damage response to insulin. The result is slow onset and reduced strength of immune response.
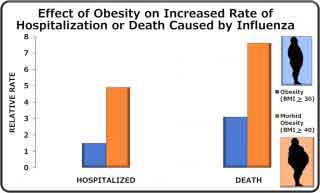 Obesity causing poor immune response to influenza was recognized during the swine flu pandemic in 2009. Response to infection was delayed, complications more severe and time to recover took longer. Also, during prolonged illness, obese patients shed more virus infecting people around them.
Obesity causing poor immune response to influenza was recognized during the swine flu pandemic in 2009. Response to infection was delayed, complications more severe and time to recover took longer. Also, during prolonged illness, obese patients shed more virus infecting people around them.
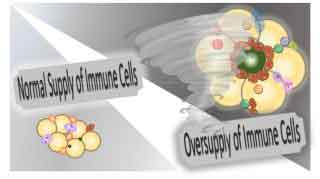 Fat tissue also has an oversupply of immune cells. Especially cells that destroy infection. More than cells that can control the immune response. Overweight, obesity and type 2 diabetes have more than safe numbers of immune cells even without infection. A new infection not quickly controlled can cause a runaway response. A storm of response that doesn’t get turned off. The result is more damage to lungs, blood vessels and brain by the immune response than by the new infection. If it doesn’t get turned off, the result is deadly.
Fat tissue also has an oversupply of immune cells. Especially cells that destroy infection. More than cells that can control the immune response. Overweight, obesity and type 2 diabetes have more than safe numbers of immune cells even without infection. A new infection not quickly controlled can cause a runaway response. A storm of response that doesn’t get turned off. The result is more damage to lungs, blood vessels and brain by the immune response than by the new infection. If it doesn’t get turned off, the result is deadly.
Weight loss with reduced fat tissue restores immunity cells to normal.
Since 2009, we realize that preventing overweight, obesity and type 2 diabetes helps prevent severe respiratory viral disease.
We’ve known for a long time that regular mild-to-moderate exercise reduces viral respiratory infection. In 2008, more than 1000 men and women in the US were studied for 12 weeks during the fall and winter. The days of illness with viral respiratory disease were 43% less in those who exercised at least 5 days/week compared to those who didn’t exercise at all.
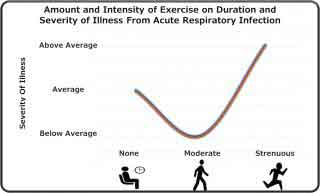 In many other studies, the results have been less clear. However, the amount and intensity of exercise of many studies shows a J-shaped response of duration and severity. Very high amounts of exercise appeared to be less effective than moderate amounts.
In many other studies, the results have been less clear. However, the amount and intensity of exercise of many studies shows a J-shaped response of duration and severity. Very high amounts of exercise appeared to be less effective than moderate amounts.
We do know that moderate exercise quickly reduces the risk of illness in overweight, obesity and type 2 diabetes. So far, studies of COVID-19 illness in China indicate that low to moderate exercise decreased mortality.
Progress detecting and treating COVID-19 has been slow. We’re not even sure that recovering from illness protects us from another infection. Another infection could be just as severe or even worse.
So far, it appears that the only way to prevent infection is to avoid contact with anyone who might be infected.
During the COVID-19 pandemic so far, 73% of patients hospitalized in New York City had obesity, type 2 diabetes or both.
We can protect ourselves from severity of illness. We can boost our immune system. By restoring and enhancing nutritional and physical fitness.
 We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com
We are pleased to share our blog articles with you, and we are always interested to hear from our readers. Our website address is: www.herdhealthcare.com




